Gastrointestinal surgery provides the most substantial and sustainable weight loss in individuals with obesity.

The procedures are collectively called bariatric (from the Greek words baros [weight] and iatrikos [medicine]) or metabolic (when the intent is cardiometabolic risk reduction surgery) and are among the most common gastrointestinal procedures.
Although bariatric and metabolic surgery procedures are used for the treatment of obesity and diabetes, it is important to distinguish between bariatric surgery and metabolic surgery. Bariatric surgery is defined as a procedure performed for weight control, while metabolic surgery is defined as gastrointestinal surgery performed to treat diabetes and metabolic syndrome. (45)
Metabolic syndrome is a group of disorders that occur together and increase the risk of heart disease, stroke, and type 2 diabetes. These disorders include high blood pressure, high blood sugar levels, excess body fat around the waist, and abnormal cholesterol or triglyceride levels.
Having just one of these disorders doesn't mean you have metabolic syndrome. But it does mean you're at higher risk for serious illness. And if you develop more of these disorders, your risk of complications, such as type 2 diabetes and heart disease, increases even further.
Bariatric surgical procedures cause weight loss by restricting the amount of food the stomach can hold, causing nutrient malabsorption, or through a combination of gastric restriction and malabsorption.
Bariatric procedures also often cause hormonal changes. Most weight-loss surgeries today are performed using minimally invasive techniques (laparoscopic surgery).
The International Federation for the Surgery of Obesity and Metabolic Diseases reported that nearly 580,000 metabolic procedures were performed worldwide in 2014. The American Society for Metabolic and Bariatric Surgery estimated that 179,000 metabolic procedures were performed in the United States in 2013 and 196,000 were performed in 2015. The American Heart Association also recognizes the growing importance of these techniques (1).
The goal of obesity treatment is to achieve and maintain a healthy weight. This improves overall health and reduces the risk of developing obesity-related complications.
Initially, a modest weight loss is ideal: between 5 and 10 percent of your total weight. This means that if you weigh 200 pounds (91 kg) and are obese according to BMI standards, you would only need to lose about 10 to 20 pounds (4.5 to 9 kg) for your health to begin to improve. However, the more weight you lose, the greater the benefits.
All weight loss programs require changes in your eating habits and increased physical activity. The treatment methods that are right for you depend on the severity of your obesity, your overall health, and your willingness to participate in the weight loss plan.
Behavior modification, sometimes called “behavioral therapy,” may include:
Vagus nerve block is another treatment for obesity. It involves implanting a device under the skin of the abdomen that sends intermittent electrical impulses to the abdominal vagus nerve, which signals the brain when the stomach feels empty or full. This new technology was approved by the FDA in 2014 for use in adults who have been unable to lose weight with a weight-loss program and who have a BMI between 35 and 45 and at least one obesity-related condition, such as type 2 diabetes.

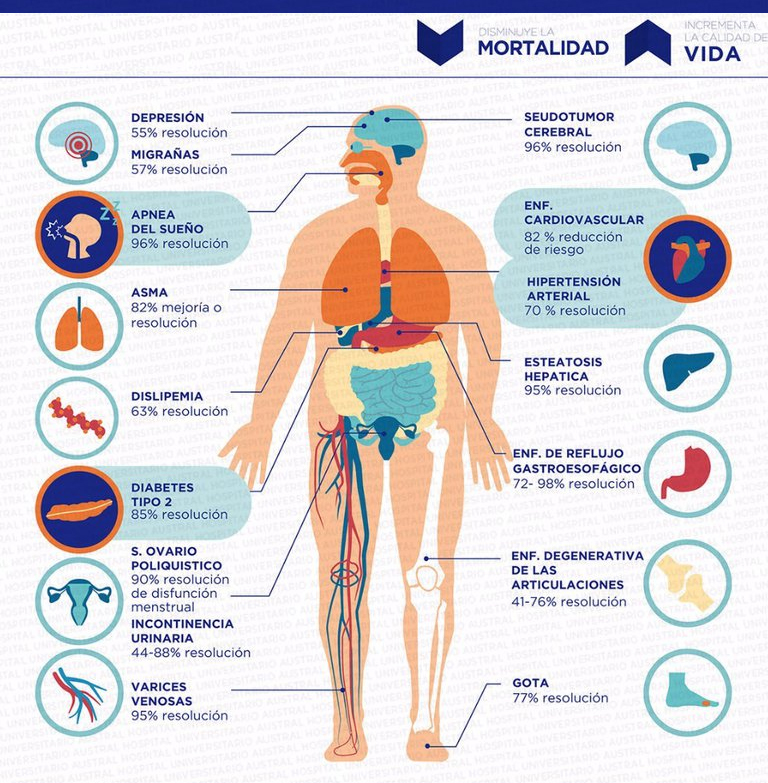
Bariatric/metabolic surgery is the most effective and long-lasting treatment for severe obesity, resulting in significant weight loss and leading to the improvement, prevention, or resolution of many related diseases, including type 2 diabetes, heart disease, hypertension, sleep apnea, and certain types of cancer (3) (4).
Indications for obesity surgery and weight-related diseases: position statements of the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) and the American Society for Metabolic and Bariatric Surgery:
• BMI ≥ 40, or more than 100 pounds overweight.
• BMI ≥ 35 and at least one or more obesity-related comorbidities, such as type II diabetes (DM2), hypertension, sleep apnea and other respiratory disorders, non-alcoholic fatty liver disease, osteoarthritis, lipid abnormalities, gastrointestinal disorders, or heart disease.
• Surgical weight loss treatment improves the components of metabolic syndrome. This applies to patients with class I obesity (BMI > 30 kg/m2) as well as to patients with higher obesity classes.
• Long-standing obesity (> 5 years)
• Proven failure of nutritional and behavioral therapy. Inability to achieve sustained, healthy weight loss over a period of time with previous weight loss efforts.
• Surgery for obesity and weight-related diseases is effective in obese patients under 18 years of age.
• Surgery for obesity and weight-related disorders is effective in obese patients over 60 years of age. Most studies conclude that the primary goal of surgery for obesity and weight-related disorders in patients over 60 years of age is to improve quality of life.
• In 2007, European interdisciplinary guidelines, in agreement with the views expressed by a document of American pediatricians, endorsed the use of surgery for obese patients younger than 18 years, supportive surgery for obesity and weight-related diseases only for patients whose BMI > 40 kg/m 2 (or > 99.5th percentile for age) with at least one comorbidity.
• Mood and anxiety disorders are not considered contraindications for surgery. Mood and anxiety symptoms should be carefully monitored both before and after surgery. Hence the importance of having a multidisciplinary team involved in the patient's treatment.
The benefits of surgery depend on the techniques performed, but in general, success in weight loss is between 68 and 85% (significant difference when compared to non-surgical treatment), resolution or improvement of diabetes in 85%, hypertension in 70%, dyslipidemia 85%, fatty liver 90%, sleep apnea 95%. This increases life expectancy by 8 years in men and 12 years in women.
After observing the metabolic benefits that surgery generated, a consensus was reached in Rome in 2003 that brought together diabetologists, cardiologists, general practitioners, and surgeons, proposing bariatric surgery to treat these metabolic diseases without having to be morbidly obese, thus giving rise to the term metabolic surgery.
Studies show that bariatric surgery can reduce a patient's risk of premature death by 30-50% (5) (6).
Patients typically lose more weight one to two years after bariatric surgery and maintain substantial weight loss with improvements in obesity-related conditions. (7) (8).
Patients can lose up to 60% of their excess weight six months after surgery, and 77% of their excess weight as early as 12 months after surgery. (9).
Most bariatric surgery patients with diabetes, hyperlipidemia, hypertension, and obstructive sleep apnea experience resolution or complete improvement (JAMA, 2004) (10)
| Condition | Disease resolved or improved | Resolved |
| Type 2 diabetes | 86% | 76.8% |
| Hypertension | 78.5% | 61.7% |
| Obstructive sleep apnea | 85.7% | 83.6% |
| Hyperlipidemia | 78.5% | 61.7% |
Achieving a BMI of less than 30 was associated with significantly higher rates of medication discontinuation for hyperlipidemia (60.7% vs. 43.2%), diabetes (insulin: 67.7% vs. 50.0%; oral agents: 78.5% vs. 64.3%), and hypertension (54.7% vs. 34.6%)
The risk of death associated with bariatric surgery is approximately 0.1% (11) and the overall probability of major complications is approximately 4% (12)
• Studies show that bariatric surgery reduces a patient's risk of premature death by 30% or more (13).
• Bariatric surgery is associated with a significant improvement in long-term survival over eight years in nearly 8,000 patients; the mortality rate was 1.5% versus 2.1% for the general population (Surgical Endoscopy, 2015) (14). Extended from eight to 14 years, the mortality rate for surgery patients was 2.5% compared to a mortality rate for the general population of 3.1%.
• Bariatric surgery helps improve or resolve more than 40 obesity-related diseases and conditions, including type 2 diabetes, heart disease, certain types of cancer, sleep apnea, high blood pressure, high cholesterol, sleep apnea, and joint problems (15)(16).
• 60% reduction in cancer mortality, with the largest reductions in breast and colon cancers (17). 56% reduction in coronary heart disease mortality, 92% reduction in type 2 diabetes mortality
• Among nearly 16,000 patients with severe obesity, all-cause mortality decreased by 40% for up to seven years after gastric bypass compared with those who did not undergo surgery (NEJM, 2007) (18).
• Deaths from any obesity-related disease decreased by 52% and were significantly lower for diabetes (92%), coronary artery disease (59%), and cancer (60%)
• Results from 2,010 patients in the Swedish Obese Subjects (SOS) study show that bariatric surgery was associated with a nearly 30% long-term reduction in overall mortality over a 20-year period compared with usual care (Journal of Internal Medicine, 2012) (19).